What is Trauma?
Trauma creates a complex blend of thought, emotional, physical, and behavioral responses, sparked by events that the brain perceives as life-threatening. Its impact extends far beyond the initial events, influencing thoughts, emotions, and behaviors immediately and over the long haul. This effect is deeply personal, shaped by an individual's history, resilience, and social environment. We often struggle with the lasting impact long after the traumatic event or period through inappropriate thoughts, out-sized emotional reactions, and behaviors that don't serve our goals but we have a hard time changing.
In the aftermath of trauma, people might face a variety of intense reactions like shock, denial, or mood swings. As time goes on, these can evolve into persistent anxiety, depression, altered self-view, and relationship issues, highlighting the profound and enduring nature of trauma.
A significant challenge with trauma is its tendency to lead to habitual brain patterns, causing individuals to repeatedly relive the traumatic experience. This cycle of distress and dysfunction can severely hinder a person's quality of life.
Recognizing and healing trauma effectively requires a comprehensive and nuanced strategy that not only addresses immediate symptoms but also focuses on retraining the brain. By incorporating brain training into the healing process, we aim to interrupt these habitual patterns, facilitating a more complete recovery. This approach underlines the importance of adopting a broad and empathetic perspective in developing therapeutic interventions for trauma.
How Trauma Affects Both Mind and Body
Trauma profoundly affects individuals, impacting not just psychological well-being but also physical health. Research underscores that the repercussions of trauma extend beyond the psychological domain, taking a tangible toll on the body. This connection between mental and physical health is critical for therapists and those seeking to understand trauma's full impact.
A key aspect of trauma's effect involves the body's stress response. Stress hormones flood the system, altering brain function, which can have significant implications for overall health. For instance, studies by Yehuda et al. (2009) and Bremner et al. (1997) have demonstrated how trauma exposure leads to elevated levels of cortisol, a primary stress hormone, which can alter brain function and affect memory, mood, and cognition.
Moreover, these hormonal changes have broader implications, including compromising the immune response. Research indicates that prolonged exposure to stress hormones can weaken the immune system, making the body more susceptible to infections and diseases. Additionally, there's emerging evidence suggesting that trauma can even reshape the architecture of our DNA, potentially leading to long-term changes in gene expression related to stress responses.
Understanding this somatic dimension of trauma highlights the importance of addressing both mind and body in the healing process. As therapists, it's crucial to integrate strategies that consider both psychological and physiological aspects of trauma. This comprehensive approach not only aids in the recovery process but also supports the overall well-being of individuals affected by trauma.
Introducing the Groundbreaking Work: The Body Keeps the Score
 Dr. Bessel van der Kolk's New York Times best seller, "The Body Keeps the Score," offers a revolutionary perspective on trauma. By weaving together neuroscience, psychology, and psychiatry, van der Kolk illuminates how trauma lodges itself in the body, advocating for integrated treatment approaches that engage the whole person.
Dr. Bessel van der Kolk's New York Times best seller, "The Body Keeps the Score," offers a revolutionary perspective on trauma. By weaving together neuroscience, psychology, and psychiatry, van der Kolk illuminates how trauma lodges itself in the body, advocating for integrated treatment approaches that engage the whole person.
Key Insights from The Body Keeps the Score
Central to van der Kolk's thesis is the idea that trauma affects the brain's ability to process emotions and memories, leading to symptoms such as flashbacks, insomnia, and hyperarousal. He argues for treatments that move beyond talk therapy to directly engage the brain's neuroplasticity, offering hope for profound healing.
The Imprint of Trauma on the Brain
Trauma profoundly impacts the brain, leaving discernible marks especially in regions responsible for managing fear, regulating emotions, and processing memories. This is substantiated by neuroimaging studies that illuminate the specific alterations trauma induces in brain structure and function. For instance, a notable study using functional MRI (fMRI) techniques showed significant differences in the amygdala and prefrontal cortex activities of individuals with trauma histories, compared to those without. These areas are crucial for fear processing and emotional control, respectively. Such findings, which are consistent with van der Kolk's discussions, emphasize the importance of developing therapeutic interventions that directly address and work towards normalizing these altered brain states. Through understanding the neural underpinnings of trauma, therapy can be more effectively tailored to help individuals reconfigure their responses to fear and emotional stimuli, facilitating a path towards recovery.
The Role of the Body in Storing and Processing Trauma
Dr. Bessel van der Kolk suggests that our bodies hold onto trauma, storing deep-seated, visceral memories of traumatic experiences. These memories are not just mental images but are embedded within our bodily sensations and can be unexpectedly triggered by sensory inputs that mirror aspects of the initial trauma, such as sounds, smells, or visuals. This phenomenon underlines the critical importance of therapeutic approaches that go beyond traditional talk therapy. By engaging the body directly through somatic experiences — practices that focus on bodily sensations and movements — therapists can help individuals process and integrate these traumatic memories more effectively. Such somatic therapies offer a pathway to healing by acknowledging and addressing the embodied nature of trauma, encouraging a more profound and holistic recovery process.
Pathways to Healing: Beyond Traditional Talk Therapy
While acknowledging the value of traditional psychotherapy, van der Kolk advocates for additional modalities that harness the body's innate capacity for healing. Techniques such as yoga, mindfulness, neurofeedback, and EMDR are highlighted as effective in engaging the body in the healing process.
By challenging conventional wisdom and advocating for a holistic approach, Dr van der Kolk has catalyzed a paradigm shift in trauma therapy. He emphasizes the integration of body-centered therapies with neurofeedback to help the brain rewire and psychotherapy, offering a comprehensive framework for healing.
Neurofeedback Explained
Demystifying Neurofeedback: The Basics
Neurofeedback is a technique similar to biofeedback that involves monitoring physiological signals and using those signals to prompt individuals to regulate their own bodily functions, aiming to transition from a state of physiological dysregulation to one of regulation. A common form of dysregulation is the body's chronic engagement in the stress response, which ideally should only activate during moments of immediate danger, known as the fight, flight, or freeze response.
Chronic activation of the stress response is linked to a decrease in immune function and is associated with various degenerative diseases, including heart disease, sleep disorders, anxiety, and depression, as recognized by the medical community.
Regulation, in this context, means adjusting the body's functions to better match its current needs and environment. When safe, this might look like a slower heart rate, relaxed muscles, deeper breathing, or, in terms of brain activity, an increase in alpha brainwaves, indicating a state of calm and readiness.
Neuroscience views the brain as a processor of information, aiming to make decisions swiftly and accurately. When made aware of its own inefficiencies, the brain has the innate ability to adjust its behavior automatically. Neurofeedback leverages this capability by providing real-time feedback on brain activity, encouraging the brain to self-optimize and enhance its functioning in response to environmental demands.
Related Article:
What is Neurofeedback Therapy?
Neurofeedback therapy is another term for neurofeedback. It is the process of learning that happens over a series of  neurofeedback sessions. Neurofeedback is not a single event because the process of change in the brain happens over time and with repetition.
neurofeedback sessions. Neurofeedback is not a single event because the process of change in the brain happens over time and with repetition.
What can be trained? The brain makes most of its decisions about internal body needs and external environmental needs unconsciously and automatically. Many of those decisions are habitual. Some are constructive and some are not. An example of an unconstructive habit is when someone yells in anger and then says, “I didn’t mean to do that. I just found myself yelling.”
That reactivity is a decision made by the brain on an unconscious level. It is an automatic reaction that most often is not the most appropriate or effective response to the current situation.
Through neurofeedback training, the individual learns to identify and change how it automatically reacts. With anything that is a habit, repetition of the new behaviour over a period of time is necessary to establish a new pattern.
How Does Neurofeedback Work?
Since the 1970s, neurofeedback technology has evolved from primarily using EEG to measure the brain's electrical activity in Hertz to incorporating MRI neurofeedback, which detects changes in blood oxygen levels to monitor neural activity.
EEG neurofeedback involves placing sensors on the scalp to capture brainwave activity through conductive paste. This data is amplified into numerical values and processed by computer software, which uses mathematical algorithms to convert these numbers into identifiable brainwave frequencies like Alpha, Beta, Theta, etc. These frequencies correspond to different mental states, such as Theta during sleep and Alpha during mental tasks.
Neurofeedback software, through its sophisticated algorithms, identifies notable shifts in brain activity. Given that neurons can transmit electrical signals at astounding speeds up to 270 miles per second, the software quickly responds with auditory or visual cues. These cues aim to guide individuals toward modifying their brain activity. The ultimate goal is to foster adaptive responses that align with immediate needs, leading to enhanced cognitive functioning, reduced impulsivity, and improved emotional regulation. This targeted feedback mechanism encourages the brain to adjust in ways that are conducive to better overall mental health and performance in real-time situations.
What Happens in a Neurofeedback Session?
In this video, Natalie Baker, Advanced NeurOptimal® Neurofeedback trainer and founder of Neurofeedback Training Co. answers the question: "How does neurofeedback work and what happens in a session?"
What Are the Different Neurofeedback Devices
Linear/Protocol Neurofeedback
Linear neurofeedback was the first generation of devices and is called EEG biofeedback systems. They work by 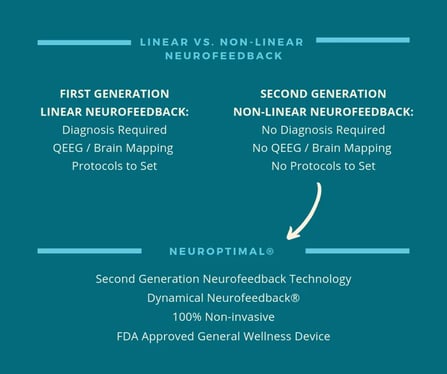 having a neurofeedback trainer first take a map of the brain’s electrical patterns. This map allows the trainer to analyze brain activity. For example, looking to see if their Theta brainwaves are low or Alpha too high in comparison with the patterns of a healthy brain. This mapping is called a qEEG- Qualitative Electroencephalography. Recorded electrical activity of the brain is used to generate a map of brain function.
having a neurofeedback trainer first take a map of the brain’s electrical patterns. This map allows the trainer to analyze brain activity. For example, looking to see if their Theta brainwaves are low or Alpha too high in comparison with the patterns of a healthy brain. This mapping is called a qEEG- Qualitative Electroencephalography. Recorded electrical activity of the brain is used to generate a map of brain function.
The map is then used as a reference point for the trainer to set protocols to help the brain to migrate towards normal and healthier brain wave patterns. When a brain map is not available, the clinician may use a diagnosis such as ADHD or anxiety to set the protocols.
Brainwave lengths represent measurements of the brain's electrical voltage, which is translated through mathematics into different frequencies. These frequencies have names, such as Theta, Beta, or Alpha, and are associated with different brain functions or states.
For example, based on your brain map, the clinician might assess that a client has too much Delta wave activity and not enough Alpha wave activity. She will create protocols to help the brain shift in those frequencies and will use client self-reports and mapping results to assess progress from session to session. A series of sessions will bring the client closer to optimal brain wellness.
With linear brain training, a client relies on the skills of the clinician, who establishes a protocol program and adjusts it over a series of sessions. Errors in adjusting frequencies- i.e. over or under the training of different frequencies- can create side effects. The skill of the clinician is very important to consider with linear neurofeedback.
Non-linear/Dynamical Neurofeedback
The second generation of neurofeedback devices arose as the speed of computing power approached the speed of the brain’s processing. The design of this system is referred to as non-linear due to the mathematical formula used, which mirrors how the brain naturally creates change. The brain’s method of change and improvement is a non-linear systemic approach.
The brain changes in a non-linear pattern and the mathematical formulation for the software of non-linear neurofeedback mirrors this pattern. Specifically, the software looks at the brain’s electrical activity or voltage and determines state change by factoring in the changes in duration, amplitude, and frequencies over time.
 Another significant difference with non-linear neurofeedback is that it does not require the trainer to set protocols. Because the speed of computing has approached brain speed, the dynamical software interacts with the brain in real-time to give it feedback so that the individual’s brain can register its own state changes and shift anything that is not optimal.
Another significant difference with non-linear neurofeedback is that it does not require the trainer to set protocols. Because the speed of computing has approached brain speed, the dynamical software interacts with the brain in real-time to give it feedback so that the individual’s brain can register its own state changes and shift anything that is not optimal.
The software takes hundreds of data points from the electrical activity measured by the EEG sensors per second. The device then uses micro-interruptions in music that is playing while the training session is running.
Hearing is the main sense perception that the brain uses to detect changes in the environment. The precisely-timed interruptions act as an alert system telling the individual brain to pay attention to two sets of information: what is happening externally in the environment and what is happening internally in the body.
The training is giving this feedback thousands of times per session. The individual brain can then use this feedback to see its own automatic choices or habits and then decide if it wants to change those patterns.
The theory behind nonlinear neurofeedback training is that over the period of training sessions the process of learning which takes place results in the most efficient and effective use of energy by the brain to respond to current environmental needs. This process of gathering current data replaces maladaptive habitual responses. Once the brain has learned this new pattern of assessing needs, the individual notices changes in mental and emotional reactions.
Neurofeedback's Transformative Effects on Trauma Survivors
Building Emotional Resilience and Stability
One of the most significant outcomes of dynamical neurofeedback for trauma survivors is the development of emotional resilience and stability. By facilitating a more regulated brain state, individuals find themselves better equipped to handle stressors and emotional triggers.
Sleep, Anxiety, and Overall Well-being Improvements
The benefits of dynamical neurofeedback extend to improved sleep quality, reduced anxiety levels, and an overall enhancement in well-being. These changes contribute to a positive feedback loop, where improvements in one area of life foster enhancements in others.
The Enduring Impact of Neurofeedback on Mental Health
The impact of dynamical neurofeedback often persists well beyond the completion of the training sessions, with many individuals experiencing lasting changes in their mental health. This enduring effect underscores the transformative potential of neurofeedback for trauma recovery.

 Dr. Bessel van der Kolk's New York Times best seller, "The Body Keeps the Score," offers a revolutionary perspective on trauma. By weaving together neuroscience, psychology, and psychiatry, van der Kolk illuminates how trauma lodges itself in the body, advocating for integrated treatment approaches that engage the whole person.
Dr. Bessel van der Kolk's New York Times best seller, "The Body Keeps the Score," offers a revolutionary perspective on trauma. By weaving together neuroscience, psychology, and psychiatry, van der Kolk illuminates how trauma lodges itself in the body, advocating for integrated treatment approaches that engage the whole person.
 neurofeedback sessions. Neurofeedback is not a single event because the process of change in the brain happens over time and with repetition.
neurofeedback sessions. Neurofeedback is not a single event because the process of change in the brain happens over time and with repetition. 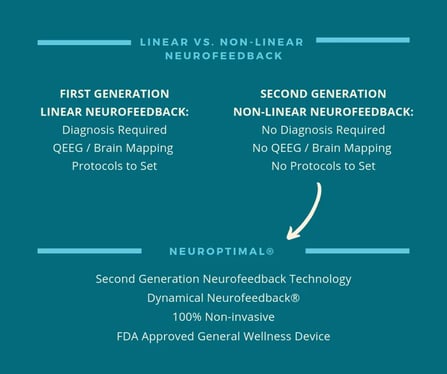 having a neurofeedback trainer first take a map of the brain’s electrical patterns. This map allows the trainer to analyze brain activity. For example, looking to see if their Theta brainwaves are low or Alpha too high in comparison with the patterns of a healthy brain. This mapping is called a qEEG- Qualitative Electroencephalography. Recorded electrical activity of the brain is used to generate a map of brain function.
having a neurofeedback trainer first take a map of the brain’s electrical patterns. This map allows the trainer to analyze brain activity. For example, looking to see if their Theta brainwaves are low or Alpha too high in comparison with the patterns of a healthy brain. This mapping is called a qEEG- Qualitative Electroencephalography. Recorded electrical activity of the brain is used to generate a map of brain function. Another significant difference with non-linear neurofeedback is that it does not require the trainer to set protocols. Because the speed of computing has approached brain speed, the dynamical software interacts with the brain in real-time to give it feedback so that the individual’s brain can register its own state changes and shift anything that is not optimal.
Another significant difference with non-linear neurofeedback is that it does not require the trainer to set protocols. Because the speed of computing has approached brain speed, the dynamical software interacts with the brain in real-time to give it feedback so that the individual’s brain can register its own state changes and shift anything that is not optimal.